An Ever "Expanding" Problem...Aortic Aneurysms
An Ever Expanding Problem, Brett Sealove, MD, FACC,RPVI
The aorta is largest artery in the body– bringing arterial (or oxygenated) blood to the body (from the brain to your legs). An aneurysm is an enlargement (dilation) of an artery and is defined as greater than 1.5 times its normal size, which in the abdominal aorta, is 3 cm or greater. This bulge can happen to any section of the aorta, and over time, tends to weaken the arterial wall which predisposes it to rupture. If the aorta bursts or ruptures, it can cause serious bleeding that often leads to abrupt death.
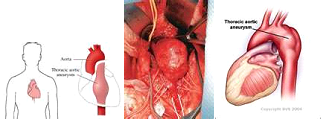
Aneurysms can form in any region of the aorta, but they are commonly seen in the belly (known as the abdominal aortic aneurysms or AAA). They can also occur in the chest (called ascending or thoracic aortic aneurysms).
Ascending (thoracic) aortic aneurysms:
Thoracic aortic aneurysms are less common than those affecting the abdominal aorta occurring in approximately 6-10 per every 100,000 people. While we do not know the etiology of many thoracic aneurysms, about 20% of those cases are linked to family history and/or linked to genetic syndromes such as Marfans, Ehlers-Danlos, and Loeys-Dietz Syndrome.
Unfortunately, there are often no signs or symptoms of aneurysms and they typically lie dormant for decades. Due to such, most aneurysms are detected incidentally when a patient undergoes a scan of his/her chest for other reasons (i.e. CT scan of the chest due to a persistent cough). On rare occasions, if the aneurysm is severely enlarged, the aorta can compress neighboring structures causing symptoms of hoarseness or difficulty swallowing. When the aneurysm results in pain, the patient may complain of a severe, sharp stabbing, pain often radiating to the back or shoulder blades.
Most commonly, ascending aortic aneurysms are followed with serial CT or MR scans to assure there is no significant progression in size. The timing of treatment vastly depends on the etiology of the aneurysm (genetic syndrome, family history, associated bicuspid aortic valve, etc). If the decision of repair takes place, conventional treatment is an open repair where the section of the aorta is replaced with an artificial graft and is surgically sewn in place. At times, depending on the location of the aneurysm, a minimally invasive procedure called a thoracic aortic endograft repair (TEVAR) may be performed where the diseased aorta is replaced by a graft deployed through a small puncture in the groin.
Abdominal aortic aneurysms (AAA):
Ruptured AAA is the 13th leading cause of death in the United States and is attributed to 15,000 deaths per year. These numbers are thought to be underestimated as often the result of rupture is death and are reported as a “heart attack” on a death certificates. AAA are more common than thoracic aortic aneurysms and are often seen in men over 65 years of age and is thought to be a degenerative process. While the true etiology is not known, it is often attributed to atherosclerosis and the risk factors that predispose to such (i.e. hypertension, smoking, etc). The most common risks are male gender, advanced age, smoking and peripheral arterial disease with others being COPD, coronary arterial disease, and hypertension. There is also a genetic link to AAA with a familial presence up to 15-20%.
Most AAA are asymptomatic and, like aneurysms in the chest, are often incidentally detected when the abdominal region is scanned for a different purpose. With that said, the abdominal aorta, unlike that in the chest, is palpable and a AAA can be detected on physical examination.
The U.S. Preventive Services Task Force recommends that men ages 65 to 75 who have ever smoked greater than 100 cigarettes have a one-time abdominal ultrasound screening for a AAA. Men ages 60 and older with a family history of abdominal aortic aneurysms should consider regular screening for the condition (often 10 years prior to their primary relative diagnosed with the disease). It should be noted that there is not enough evidence to determine if women with similar risks (including family history of an abdominal aortic aneurysm) would benefit from similar screenings as men and should be considered on an individual basis.
Likely an aneurysm in the thoracic, close surveillance is absolutely imperative with correction of the aneurysm depending on rate of expansion, size, and etiology. Historically, most AAA enlarge ~0.2-0.8 cm/year and are most susceptible in regions of high tensile stress (hence the need for aggressive blood pressure control). The goal of treatment is to prevent aneurysm rupture but also the associated risk factors mentioned above as well as other associated atherosclerotic disease states. Surgical repair for AAA is generally done when the aneurysm reaches 5-5.5 cm in size (or sooner if it grows at a rapid pace). Over the years, and with improved technology and techniques, an endovascular approach called EVAR treats the diseased AAA segment. In this procedure, a mess graft (compressed and placed within a sheathed scaffold) is placed within the diseased segment and is anchored with small pins or hooks and subsequently prevents the diseased aneurysm from expanding. An open repair replaces the aneurysmal segment with a graft and is often reserved for those with complicated AAA (i.e. involving the renal arteries).
While no specific lifestyle or diet can prevent aneurysms from forming, close blood pressure control is pivotal to minimize the tensile force on the aorta and minimize its risk of expanding. Smoking cessation, sugar control, and modest aerobic fitness (with minimal isometric exercises) can also help minimize aneurysmal growth. But perhaps most importantly, if present, it is essential that one enters a surveillance program under the guidance of a supervised physician and notifies their family members to be screened for this often silent (and potentially) deadly disease.